The uniting purpose of the Alliance for Addiction Payment Reform (Alliance) is to advocate and support the transformation of payment and delivery of addiction health services through the integration of early intervention, treatment, and recovery resources, as well as key operational components, measures, payment methodologies, tools, and practice guidelines. What are the most relevant “measures” to track? How is recovery progress and success defined? Who determines which treatment outcomes should be incorporated into value-based reimbursement methodologies, and when will these outcomes incentivize recovery? These are all important questions to consider when deploying value-based reimbursement mechanisms, ideally reflecting patient-centered measures.
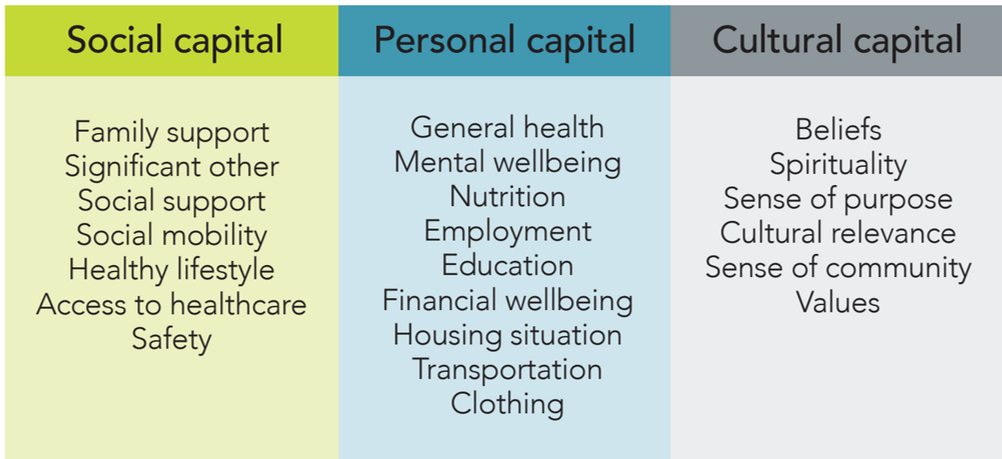
One of the frameworks that has been designed with these questions in mind is the Recovery Capital Index (RCI). At its core, the RCI seeks to incorporate a comprehensive measure of subjective recovery, outcomes, and well-being through personal, social, and cultural capital. These three areas consider elements such as general health, housing, social support, access to health care, a sense of purpose, and spirituality. Since its introduction, the RCI has evolved into a well-researched and validated tool accepted by the Joint Commission for the purpose of conducting measurement-based care.
To learn more about the RCI, I connected with Alliance participant and architect of the RCI, David Whitesock of Commonly Well, a behavioral health analytics and care experience firm. Specifically, I focused our conversation on how the RCI came to fruition and the value that it has demonstrated to organizations that are committed to person-centered outcomes in substance use disorder (SUD) treatment.
Eric (Alliance for Addiction Payment Reform): David, thanks so much for meeting with me regarding the Recovery Capital Index. First, can you take a moment to describe the RCI framework that you’ve developed for collecting meaningful, subjective measurements of recovery outcomes?

David Whitesock, Founder and CEO, Commonly Well
David (Commonly Well): Thanks for the opportunity to have this important conversation, Eric. The development of the RCI, both as a measure and a framework for measuring the complexity of recovery, began as a simple but challenging prompt. In 2012, I was working for a peer support organization called Face It TOGETHER. The local integrated health system challenged us to build data and evidence for our success. I happened to be in the office that day when our two co-founders were given this challenge. Charlie walked over to my desk and said, “David, you have 30 days to figure out how to measure recovery.”
Like most, my personal and general reference for “recovery” was sobriety. But our experience coaching and the ultimate literature review told a different, more complicated story. Two concepts caught my attention. The first was the concept of recovery capital, as described by William Cloud and Bob Granfield. They recognized there was way more going on, especially with those they said experienced “natural recovery” or a process that did not involve clinical care.
The second concept was the notion of social progress. Just as I was diving into the writings of William White, David Best and Alexandre Laudet, a group from Harvard and MIT were creating a social alternative to the economically focused gross domestic product. The Social Progress Imperative was an initiative that brought together available non-economic data that describes the social health and progress of a nation. Their framework around basic needs, foundations of well-being, and opportunity helped give some order to varying domains of recovery capital.
Eric: How has the RCI evolved over time?
David: The RCI started as a 121-item questionnaire. It was kind of a mess. Since no recovery capital scale or measure had been validated at the time, we had to test a lot of different questions and methods. One of the first things we learned from client feedback was that they liked when we organized the questions into similar groups. For example, it wasn’t enough to indicate that some questions were social capital questions – that was too broad. But when we identified a few questions as relating to your significant other or social support, we started to get stronger answers.
With the help of experts in the field like Dr. Sara Dolan at Baylor University, we narrowed the RCI down to 68 items, landed on statements over questions, and clearly aligned all items into describable indicators, components, and domains, giving the measure a strong framework for scoring and presentation.
More importantly, in that narrowing of the RCI to 68 items, we intentionally left out items specifically related to a person’s consumption of alcohol or drugs and their attendance in recovery support services or meetings. As we gathered more and more completions, it became clear that scoring use and involvement in what we call recovery-specific activities penalized pathways, resulting in spectacular success and quality of life.
Aside from the original validation of the 68-item RCI, we’ve developed statistically determined shorter versions at 36 and 10 items. The RCI is translated into Spanish and Creole. And we’ve developed an alternate version of the RCI, converting the recovery capital language to a resilience capital framing, allowing us to deploy the exact same measure across wider audiences and population types.
Eric: What are some examples of organizational success incorporating the RCI into their clinical outcomes measure sets?
David: Thanks for asking this question, as it lets me shine a light on those who are doing the real work. We have been working with Palm Beach County since late 2019. The RCI was adopted to be a shared performance measure in the middle of the County’s emerging Recovery Oriented System of Care. Twelve agencies across the continuum have adopted the RCI. Most recently, Florida Atlantic University’s Dr. Heather Howard completed an analysis of RCI data related to a reentry population. We’ve learned that the greatest contributor to housing stability at 90 days is social support and that feeling unsafe in one’s home, work, or community is predictive of rearrest. Agencies are now incorporating these learnings where appropriate.
Oregon Recovery and Treatment Centers, or ORTC, operates seven MAT clinics across Oregon and Washington states. Generally, this is a challenging population. Clinical directors didn’t really know what contributed to treatment adherence. A few insights are emerging and are being applied where appropriate. For example, strong social support or overall social capital is the greatest contributor to treatment adherence. Closely aligned is being both employed and satisfied with employment.
We don’t view employment on its face as positive recovery capital. In fact, our data often distinguishes greatly between employment status (part-time versus full-time) and employment satisfaction (like my work versus respected at work). In the case of ORTC, scores in employment (satisfied/respected) were one of the greatest contributors to increases in overall recovery capital AND treatment adherence.
In the case of both Palm Beach County and ORTC, the RCI is adding nuance to the measure sets and is driving policy, protocols, and even payment frameworks.
Eric: Given what you know about the mission of the Alliance and our commitment to addiction treatment payment reform, how can the RCI complement efforts to shift to value-based reimbursement methodologies in the SUD treatment space?
David: The shift to value-based or performance-based reimbursement is critical to shepherding an improvement in the overall quality of care industry-wide. I see the RCI as a strong complement to the Alliance’s efforts by adding the patient’s voice to the equation. Here’s what I mean.
We have a lot of patient-reported outcome measures, such as the GAD-7 or the PHQ-9. These measures are clinical and proximal to the person’s diagnosis. These measures and other clinical or operational metrics typically included in value-based care models generally exclude a wide range of externalities affecting patient outcomes. Value-based or performance-based care must function on a longer timeline, which the Alliance’s alternative payment model reflects. Since the RCI was designed and has strength as a longitudinal measure, it can sufficiently monitor a person’s social determinants or externalities that may limit the effectiveness or stickiness of a particular treatment.
In other words, the RCI provides a broad-based mapping of those externalities as observed by patients in a community. We can establish a baseline from which general value-based care models can be appropriately adjusted to account for communities with less foundational recovery capital (because recovery capital isn’t just intrinsic to the person). I believe the RCI can help establish more equitable value-based care models over time.
Eric: What have been some of your biggest challenges with promulgating the RCI?
David: With anything in our field, introducing something new takes time. William White and Robert Granfield introduced recovery capital 25 years ago, and yet, it’s not widely known or embraced by clinicians. So, that’s a challenge.
Another challenge we experience is a general lack of data literacy. The RCI is a complex questionnaire. There are a lot of ways we can present the results, both at the patient and aggregate levels. We’ve worked with world-class data visualizers to meet the audience where they are, but there remain some underlying barriers to understanding data and feeling comfortable using it in real-time care.
Which leads us to the last big challenge: technology. There is a lot of digital health technology emerging in our field. Organizations are using a multitude of systems, most that don’t synch with one another or actively compete with one another. While I don’t believe in all-in-one solutions, mostly because they price out 90 percent of the field, I do believe in a thoughtful digital and data strategy. Health care generally has understood what this means for almost 20 years now, behavioral health is just now catching up. This is why, for nearly all of our customers, we are not just a software vendor but function as the organization’s fractional Chief Data Officer or Program Evaluator. Whether it’s the RCI or some of the standard clinical measures, even some of the most sophisticated organizations need data audits and data strategies. We’re happy to serve in this capacity because we believe that the patient’s voice lives in most of the data that’s captured and that voice requires a prominent role in how care is designed, delivered, and paid for.
Eric: What are some final considerations you would like to pass along to our Alliance participants?
David: My final thought to Alliance participants is that you don’t need to wait for some blessing on high to get started with data or think you’re not ready for value-based care. I intentionally use the phrase performance-based care instead of value-based to get this point across. Ask yourself or your leadership team: “What determines positive performance in our clinic or programs?” Come up with the answers. Let’s say one of them is “building recovery capital.” Adopt a recovery capital measure and apply it conservatively but consistently. Gather as much data as you can for as long as you can – don’t worry about applying the insights right away. Do one thing at a time: grow the muscle of data capture. Once you have six to nine months of data, look at it. Did the numbers go up or down? Depending on the result, what do you do to adjust?
Look out, you are now performance-based.
I know that is a massive over-simplification, especially for this esteemed audience, but the majority of the field is really struggling to do what some take for granted. A return to the basics and a move toward simplification before sophistication is warranted if we want to get value-based care right and make it inclusive to most in our field.
Eric: David, thanks for your thoughtful responses to this important conversation. Your comments have given us a great deal to consider when considering the RCI and how it may complement our collective efforts to move toward payment innovations that embrace holistic, patient-centered outcomes measures.
If you would like to learn more about the RCI, David Whitesock will be our featured spotlight speaker during our upcoming virtual learning collaborative meeting scheduled for 3/13/24, from 3:00-4:30pm EST. If you are interested in participating in this or any of the quarterly Alliance meetings, visit www.incentivizerecovery.org and select the quarterly meetings link to add yourself to the participant list. If you encounter any issues with this process, please email Eric Bailly at eric@thirdhorizonstrategies.com.
For any questions or to join the conversation and connect with Alliance, please fill out this form and follow our public LinkedIn page.
The Alliance for Addiction Payment Reform (Alliance) is a national multi-sector alliance of health care industry leaders – including payers, health systems, recovery service providers, and subject matter experts – dedicated to aligning incentives and establishing a structure that promotes the type of integration and patient care capable of producing improved outcomes for patients, payers, and health systems. The Alliance brings together clinical, addiction, information technology, primary care, social, regulatory, and policy expertise and has logged hundreds of hours of workgroup meetings, ratifying consensus principles and outputs.
Commonly Well (www.commonlywell.com): is a behavioral health analytics firm that serves addiction treatment, mental health, recovery support, and public health entities with data and communications software and services that improve insights, determine outcomes, and enhance the patient experience. At the heart of Commonly Well’s work is a recovery intelligence model that measures total well-being by engaging participants through secure text messaging and using a battering of scientifically validated assessments, including the Recovery Capital Index.